The doctor will decide which type of bariatric surgery to be performed that is suitable to the patient. There are different types of bariatric surgeries:
 1. Gastric bypass
1. Gastric bypass
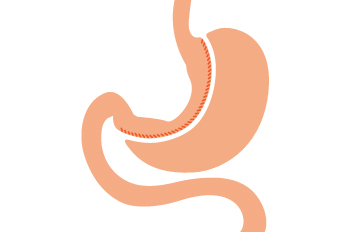
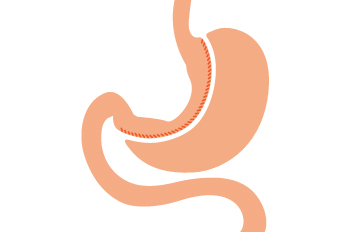
It is also called as Roux-en-Y gastric bypass. Gastric bypass is considered as the ‘gold standard’ of weight loss surgery. This procedure involves two steps.
- First, the surgeon creates a small pouch at the top of the stomach by stapling section of the stomach together, or vertical banding. The small pouch is about the size of a walnut, which can hold only about an ounce of food. Hence, the person eats less and feels full soon.
- Secondly, the surgeon cuts the small intestine and connects it to the newly created pouch. The rest of the stomach and upper part of the small intestine is then connected farther down to the lower portion of the small intestine. This enables the stomach acids and digestive juices from the bypassed stomach and first portion of small intestine to flow into the lower portion of the small intestine.
Gastric bypass helps in the absorption of fewer nutrients and calories, as food bypasses a portion of the small intestine (where most of the absorption takes place). This procedure also causes changes in gut hormones and gut bacteria that reduces appetite and enhance satiety. The changes in the gut hormones also reverse one of the primary mechanisms by which obesity induces type 2 diabetes. Gastric bypass is an irreversible procedure and leads to a rapid weight loss.
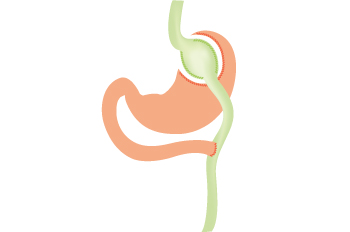
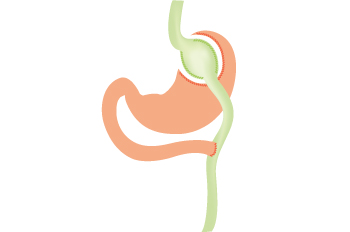
2. Sleeve gastrectomy (Gastric sleeve)
It is also called as gastric sleeve or vertical sleeve gastrectomy. In this procedure, the surgeon removes almost 80% of the stomach, leaving only a banana-shaped section that is closed with staples. The newly created stomach pouch holds only a small amount of food consumed, so that the person eats less and feels full sooner. As most of the stomach is removed, gut hormones and gut bacteria are affected leading to reduced appetite, satiety. Gut hormones also has an impact on the blood sugar control.
Sleeve gastrectomy is not reversible, as most of the stomach is permanently removed. This procedure is similar to the gastric bypass and is effective in improving type 2 diabetes too.
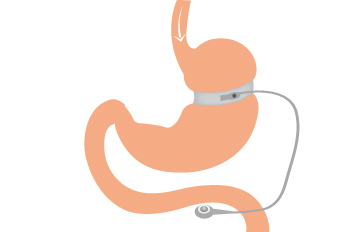
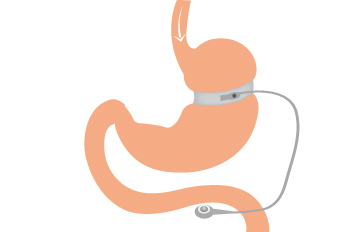
3. Adjustable Gastric Band
In this procedure, the surgeon places an inflatable band around the upper part of the stomach to create a small pouch. This small pouch opens into the lower stomach through a small channel or opening. The band is connected to the port placed under the skin through a tube. The size of the stomach opening can be adjusted by filling the band with sterile saline, which is injected through a port. The pouch holds only small amounts of food, which makes the person to eat less and feel full soon. The feeling of fullness depends upon the size of the opening.
As this procedure does not involve removal of any part of the digestive tract, it doesn't reduce the absorption of calories and nutrients. Due to its simplicity, this procedure is most commonly used. But, it may lead to less weight loss compared to other procedures; and the patient needs several follow-up visits after surgery to adjust the size of the band opening.
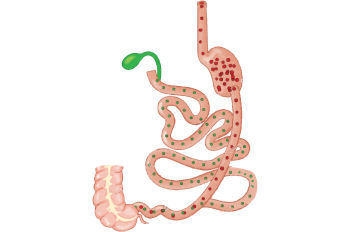
4. Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
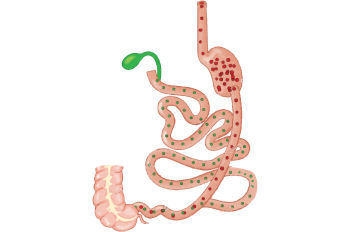
This procedure initially involves removal of most of the stomach similar to the gastric sleeve procedure to create a small pouch. Then the valve that releases food into the small intestine along with the first part of the small intestine (duodenum) is cut off or separated from the lower portion of the small intestine. The pouch is then connected to the lower portion of the small intestine. The surgeon reattaches the bypassed section with the lower portion of the small intestine, which is called as duodenal switch. This procedure allows the bile and pancreatic digestive juices of the bypassed intestine to flow into lower portion of the small intestine. These digestive juices are required for the breakdown and absorption of proteins and fats. This is called as biliopancreatic diversion.
The small pouch created holds only small amounts of food. This procedure also affects gut hormones that impacts hunger, satiety and blood sugar control. As most of the small intestine is bypassed, there will be malabsorption of vitamins and nutrients. This procedure is effective for type 2 diabetic patients and also for people who have a body mass index of >50kg/m². This surgery is mostly associated with risks after surgery, so surgeons generally do not prefer this procedure even though it is effective in weight loss.




 1. Gastric bypass
1. Gastric bypass